How is an ankle sprain caused?
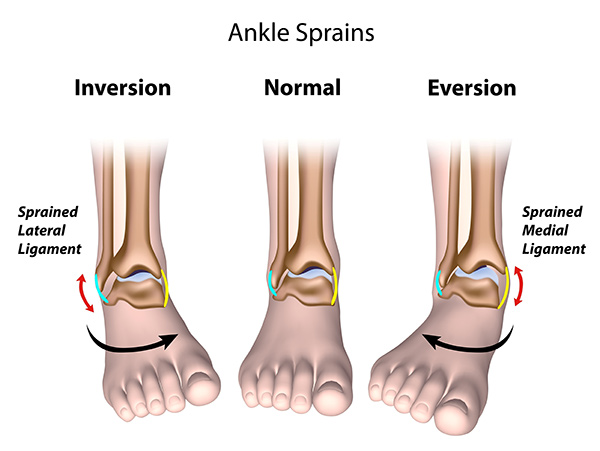
An ankle sprain is one of the most common injuries around the foot and ankle. ‘Sprain’ refers to stretching of the ligaments that provide stability to the ankle. Different mechanisms of injury include an ‘inversion’ injury when the ankle rolls inside, ‘eversion’ injury when it rolls outside or a twisting injury as shown in the illustration below.
Which are the ligaments around the ankle joint?
The ankle ligaments are divided into 3 major groups based on their anatomic position. These are the lateral ligaments which are on the outer side of the ankle, the medial ligaments on the inner side of the ankle, and lastly, the ligaments that join the tibia bone and the fibula bone, the so-called ‘syndesmosis’. Of these, lateral ligament sprains are by far the most common and typically involve injury to the Anterior talofibular ligament (ATFL) and Calcaneofibular ligament (CFL). Conversely, injury to the inner ankle ligament, called the Deltoid, is much less common.
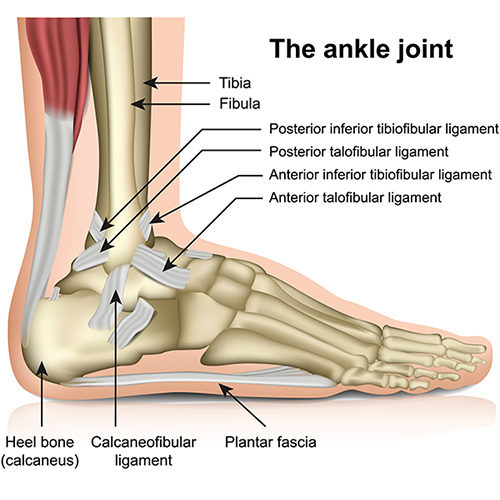
The clinical picture above shows the location of the ankle ligaments that are commonly sprained. These are the anterior talofibular ligament and the calcaneofibular ligament.
What are the symptoms?
The common presentation includes pain, swelling, difficulty in weight-bearing and bruising. The bruising can be severe and involve most of the ankle, foot as well as lower leg. Over the longer term, the ankle may feel ‘loose’ and give way to twisting or turning, or when trying to play sport, climb up and downstairs. You may feel that you are not able to ‘trust’ the ankle and rely on using the other ankle more or place more weight through your other leg. Furthermore, in approximately 8-10% of patients suffering a severe ankle sprain, there will be associated injuries to the cartilage within the ankle joint itself, that may lead to residual symptoms.
Assessment
Your symptoms and a medical examination will be performed by Mr Davda to determine the type of treatment that will be most appropriate for you. Certain risk factors such as the shape of the heel bone or generalised ligament laxity will be examined. Conditions such as diabetes may be present and affect the method of treatment.
Imaging
Weight-bearing x-rays will be taken to assess the ankle joint and exclude any other injury. Further evaluation with an MRI may be required to examine the ankle bones and surrounding soft tissue such as tendons and cartilage in greater detail.
What treatment is available?
Conservative management
This is usually successful for the majority of patients. Simple ankle sprains can be managed initially with rest, ice, compression with a Tubigrip and elevation above the level of the heart (by resting the leg on three pillows for example). Simple pain killers, taken regularly, such as ibuprofen will help reduce inflammation and swelling. Your consultant may suggest using a walking boot or ankle brace for 3-6 weeks following the injury. This helps in healing the ligaments, prevent overstretching and possible re-injury. The key to successful rehabilitation, once the initial symptoms settle, is a guided physiotherapy programme. These will work on improving ankle range of movement, strength and balance (known as ‘proprioception’). Shockwave or ultrasound therapy can be an alternative when physiotherapy has not been fully successful. Occasionally, residual scar tissue from the injury and subsequent instability may cause ankle pain. This can be treated with an ankle injection, containing both local anaesthetic and steroid.
Surgical management
This is required if a 3-6 month course of physiotherapy does not improve ankle stability Indications include the ankle giving way or when there are combined injuries of the articular cartilage of the ankle joint. In most cases, reconstruction is deemed appropriate for the injury of the lateral ankle ligaments, which are the Anterior Talofibular Ligament and the Calcaneofibular Ligament. Repair or reconstruction of the medial ankle ligament which is called deltoid ligament is performed in very selected cases.
Surgical treatment
Before surgery
Your fitness for surgery will be reassessed in our pre-assessment clinic, which usually takes place prior to the date of operation. Blood tests and further investigations of the heart and lungs may be required to ensure you are fit to have a general anaesthetic. If you live alone, we will liaise with your GP and social services to ensure that care is in place to look after you following surgery. Occasionally, you may need to spend a few more days in hospital whilst the services are being organised.
We kindly ask that you contact us if you suffer an insect bite, cut or bruise to the symptomatic foot in the period leading up to your surgery, or if you have been unwell. Any injury to the skin in the area of your intended surgery can increase the risk of infection. You may need reassessment and surgery reorganised for another time.
On the day of the surgery
You will be seen by your consultant or a team member to check your consent and mark the leg. Ankle ligament reconstruction surgery is typically performed under general anaesthetic, which can be discussed with your anaesthetist.
In most cases of ankle ligament reconstruction surgery, you will be able to go home the same day. Sometimes, it is necessary to spend a night in the hospital depending on your general health and immediate recovery from the operation. Local anaesthetic is also applied at the time of surgery to provide pain relief and numb the foot. This can last for up to a day after.
The operation
Reconstruction of the lateral ankle ligament can be either anatomic or non-anatomic. Anatomic reconstruction involves tightening the stretched outer ligaments known as the Brostrom procedure. The ligaments are double breasted and stabilised with sutures that are anchored to the fibula bone. Non-anatomic reconstruction is performed by the use of a synthetic graft in the form of an artificial ligament and is reserved for specific revision cases.
After the operation
It is not uncommon for the wound to bleed a little and stain the bandaging, particularly when standing for the first time after the operation. You will be immobilised with a below-knee cast which should remain in place for 2 weeks until you are seen by Mr Davda in the clinic. You are advised to elevate the foot on 2-3 pillows as much as possible, and limit the amount you walk to as little as practically needed. This will help reduce the swelling in the foot and promote healing of the wound. Whilst in cast you will be asked to take an injection on a daily basis to reduce the risk of clot in the leg or lung. You will be shown how to self-administer this on the ward prior to discharge. Further information on how to administer blood thinning medication is available here.
Recovery
At about two weeks following surgery, you will be seen in the clinic when the wound is inspected for a fresh cast. You will continue to be non-weight bearing for a further 4 weeks. At that point, you will be able to start weight-bearing, be placed into a brace and physiotherapy will commence.
Common Questions
When can I drive?
Patients having had their left foot operated on will be able to drive an automatic car within two weeks. Those who have had an operation on the right side will be able to drive after the boot or brace is removed, around 8 weeks after the procedure. You are advised to contact your insurance company to ensure you are covered to drive. Flying is best avoided for 6 weeks following surgery.
When can I go back to work?
This will depend on the type of work you do. For example, if you have a desk job you may be able to return to work after two weeks provided you are able to rest and elevate your foot whilst sitting. If you do a physically demanding job, you will need 12 weeks off.
When can I return to sport?
You can usually return to sports between three and six months from the date of surgery. Non-impact exercises such as swimming, cycling and elliptical machine are a good way of building stamina and strength following surgery and minimise the likely hood of ‘undoing’ surgery.
Complications
Swelling
This is very common after surgery. It is a side effect, rather than a complication, and can take up to a year to recover. You may need a shoe size slightly larger than you normally wear during this period.
Infection
This can occur in a small percentage of patients. If this is the case, it is possible that further surgery may be required to remove infected bone or screws. Minor infections are common and normally settle after a short course of antibiotics.
Numbness and tingling
This occurs at the surgical site, as a result of minor nerve damage and usually recovers over the course of six months.
Stiffness
This can occur in the ankle joint and normally improves with physiotherapy
Recurrence
Symptoms may recur despite conservative or surgical management.
Blood clots
A clot in the calf of the operated foot (known as deep vein thrombosis or DVT), or a clot in the lung (known as pulmonary embolus or PE) is rare. Please inform the team if you have had a DVT or PE before, or if you have a family history of clotting disorders. You may require a short course of a blood-thinning injection if this is the case, or if we are operating on both feet at the same time.
