What is Plantar Fasciitis?
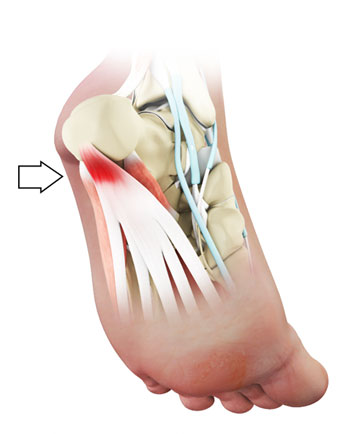
Plantar fasciitis is one of the most common causes of heel pain. It can affect both active and sedentary individuals. The plantar fascia is a thick band of tissue under the skin of the sole of the foot. It provides protection to the foot when walking and is involved in the mechanism to give a normal walking pattern.
How is plantar fasciitis caused?
Current evidence suggests that this is a degenerative condition due to the hardening of the normal plantar fascia rendering it more prone to microtears. The micro tearing leads to an inflammatory response that produces pain. Risk factors include a tight Calf Muscle, high activity levels (such as running, or a job involving lots of standing and walking), and increased body weight.What are the symptoms?
Symptoms are typically worse during the first steps in the morning and tend to ease with mobilisation. Prolonged standing and walking aggravate the pain and the initially intermittent pain can progress to a continuous tenderness. It can recur as the day progresses. The condition is typically self-limiting and in most cases will heal over the matter of 6 -9 months.
Assessment
Your symptoms and a medical examination will determine the type of treatment that will be most appropriate for you. Conditions such as rheumatoid arthritis and diabetes may be present and affect the method of treatment Mr Davda provides. Burning pain is not typical of plantar fasciitis and may suggest irritation of a local nerve in the foot. Other sources of heel pain include wear and tear of the Achilles tendon, and occasionally irritation of a nerve in the lower back, so called ‘sciatica’. Clinical examination of the symptomatic foot and investigations such as an xray, ultrasound or MRI might be necessary before a management plan is set.
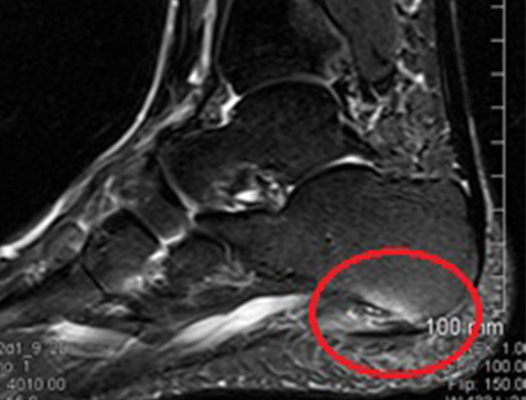
This MRI image is of the heel. The red circle outlines the fluid found around the plantar fascia.
Importantly, a heel spur is not related to plantar fasciitis. This is often seen on an xray and thought to be the cause of plantar fascia symptoms. It is in fact anatomically distinct. Many patients will have a heel spur on xay and not have symptoms, while many will have symptoms and not have a spur.
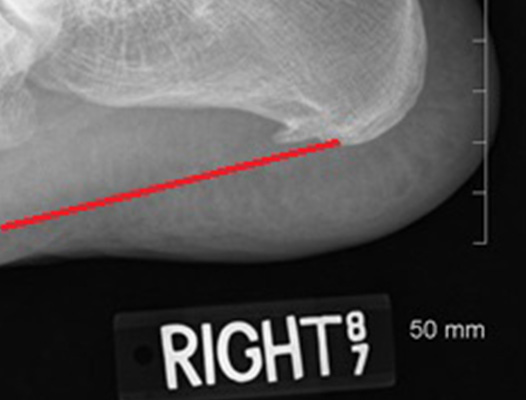
The xray above shows a large heel spur. The plantar fascia is represented by the red line and is anatomically distinct from the spur itself.
Treatment
The vast majority of cases can be managed with conservative measures. This includes rest, analgesia, avoidance of sporting activities for the period of treatment, use of appropriate footwear, avoidance of walking barefoot, and stretching exercises:
Calf stretching
Regular daily calf stretching performed over a 6 to 8 week period will alleviate plantar fasciitis in almost 90% of patients.It should be done with the knee straight so that the calf muscle is stretched, as this is the muscle that is tight. It should be performed on both sides and important that the stretches are done daily. The exercises are shown here.
Plantar Fascia Specific Stretch
Equally good results can be obtained with a formal plantar fascia stretch. Plantar fascia specific stretching has been found to provide symptomatic relief for the majority of patients.
This is done in a seated position and includes crossing the affected leg over the other leg. Using the hand on your affected side, take hold of your affected foot and pull your toes back towards your shin. This creates tension/stretch in the arch of the foot/plantar fascia. Check for the appropriate stretch position by gently rubbing the thumb of your unaffected side from left to right over the arch of the affected foot. The plantar fascia should feel firm, like a guitar string. The stretch position should be held for 10 seconds and repeated 10 times. The timing of when this is performed is important. It should be done prior to the first step in the morning and during the day before standing after prolonged inactivity. Most patients perform the stretch 4-5 times during the day for the first month, and then on a semi-regular basis (3-4 times per week). Decreased pain, with improvement of about 25-50% is expected at 6 weeks, with resolution of symptoms over 3-6 months.
With resolution of the heel pain symptoms, it is important to continue calf stretching and plantar fascia stretching on a semi-regular basis (3-4 times per week), so as to minimise the risk of recurrence.
Strassburg Sock
This can be worn at night and provides passive stretch of the plantar fascia.

Over-the-counter insoles
A soft, over-the-counter orthotic with an accommodating arch support has proven to be helpful in the management of plantar fascia symptoms. A gel heel insert may also help.
Comfort Shoes.
Shoes with a stiff sole, a rocker-bottom contour, and a comfortable leather upper, combined with an over-the-counter orthotic or a padded heel can be very helpful in the treatment of plantar fasciitis.
Activity Modification
Any activity that has recently been started, such as a new running routine or a new exercise at the gym, that may have increased loading through the heel area, should be stopped on a temporary basis until the symptoms have resolved.
Plantar Fascia Night Splint
A night splint keeps the ankle in a neutral position while sleeping. This stretches the calf muscle, Achilles tendon and plantar fascia. It can be very helpful in alleviating the significant morning symptoms and can be ordered online or even obtained in some chemists. This splint is worn nightly for 1-3 weeks, until the cycle of pain is broken. Furthermore, this splinting can be reinstituted for a short period of time if symptoms recur.


Weight Loss
Loosing weight has been proven to improve plantar fascia symptoms.
Interventional Treatment
For plantar fasciitis that is resistant to the measures described above, there are a number of interventional options Firstly, a local injection of corticosteroids and local anaesthetic may help to break the cycle of pain and inflammation. This is usually delivered under image guidance using ultrasound. Other forms of treatment include PRP (Plasma-Rich Protein) injections or shockwave therapy. This can be discussed in more detail in clinic.
Surgery
About 90% of patients will respond to appropriate non-operative treatment measures over a period of 3-6 months. Surgery is a treatment option for patients with persistent symptoms, but is NOT recommended unless a patient has failed a minimum of 6-9 months of appropriate non-operative treatment.
Surgical management is indicated in patients with plantar fasciitis who have been have diagnosed with a tight calf muscle. The proposed surgery includes release of the tight fascia through a small incision at the back of the calf. The surgery is described in greater detail here.
Other surgical procedures
Partial Plantar Fasciectomy
This involves removal of the injured area of the plantar fascia, either endoscopically or through the small incision. This is then followed by a 6-week period of relative rest and stretching. Although this procedure has produced good results, it can increase the risk of a rupture of the plantar fascia, with resulting profound flatfoot deformity and an increase in symptoms. It is not often performed due to the risks and is often seen as a procedure of last resort.
