What is Achilles tendonitis?
The Achilles tendon is the largest and strongest tendon in the body. It connects the calf muscles to your heel bone, providing the power to walk, run, climb stairs, jump, and stand on tiptoes. Achilles tendonitis is a general term that describes inflammation of the tendon, causing pain. It is associated with overuse or wear or tear of the tendon. The latter is more appropriately termed ‘tendinopathy’ of which there are two patterns:
Non-insertional Achilles Tendinopathy
In non-insertional Achilles tendinopathy, wear and tear occur in the middle portion tendon between the calf muscle and its attachment in the heel. This is typically located 2-6 cm above the insertion of the Achilles tendon to heel bone. The tendon fibres break down with tiny tears, swell and thickens in response.
Insertional Achilles Tendinopathy
Insertional Achilles tendinopathy involves the lower portion of the heel, where the tendon attaches to the heel bone.

The Achilles tendon connects the calf muscle to the heel bone as shown in the picture above.
What causes Achilles tendinopathy?
Achilles tendinopathy is usually not related to a single injury. The problem results from repetitive stress to the tendon and is multifactorial
- A change in everyday activities from the normal, such as a more active job
- A sudden increase in the amount or intensity of exercise
- Tight calf muscle. This condition is described in greater detail here
- Bone growth around the heel bone can cause irritation and rubbing of the tendon
- Use of certain antibiotics such as quinolones
What are the symptoms of Achilles tendinopathy?
Common symptoms include:
- Pain and stiffness along the Achilles tendon and back of the ankle in the morning
- Pain on the back of the heel that worsens with activity
- Severe pain after exercising
- Thickening and enlargement of the tendon
- Swelling which is present all the time and gets worse throughout the day with activity
If you experience a sudden “pop” in the back of your calf or heel, you may have torn your Achilles tendon.
Assessment
A thorough history of your symptoms will be taken by Mr Davda and a clinical examination will be performed. Specific features of Achilles tendinopathy that will be sought are:
- Swelling and thickening along the Achilles tendon or at the back of your heel
- The point of maximum tenderness. Pain in the middle of the tendon indicated ‘non-insertional tendinopathy’, whereas tenderness to the back of heel at the lower part of the tendon indicates insertional tendinopathy
- Bony spurs at the back of the heel
- Tight Achilles tendon
Imaging
X-rays
These provide clear images of the ankle and heel bone. These images may show calcium deposits in the Achilles tendon and if a bump is present along the back edge of the heel bone, known as a Haglund’s deformity.

The x-ray above shows an enlargement of the heel bone, known as a Haglund’s deformity.
Magnetic Resonance Imaging (MRI)
Unlike an X-ray, an MRI scan shows soft tissues such as tendons and ligaments in detail. The severity of degeneration and overall quality of the tendon can be assessed. This allows further planning of management, and if needed, the surgical procedure that is best suited.


The MRI above is of the same patient who had the x-ray earlier. Here, the bone rubs on the inner surface of the tendon, and is associated with fraying of the tendon and a build up of fluid, known as a retrocalcaneal bursa.
What are the treatment options?
Conservative Treatment
In most cases, nonsurgical treatment options will provide pain relief, although it may take 3 to 6 months for symptoms to completely subside.
Rest
The first step in reducing pain is to decrease or even stop the activities that make the pain worse.
Ice
Placing ice on the most painful area of the Achilles tendon is helpful and can be done as needed throughout the day. This can be done for up to 20 minutes.
Non-steroidal anti-inflammatory medication
Drugs such as ibuprofen and naproxen reduce pain and swelling.
Exercise
The following exercises can help to strengthen the calf muscles and reduce stress on the Achilles tendon.
- Calf stretching
- Physical Therapy including Eccentric Strengthening Protocol
These exercises can be found in the Achilles stretching section, with videos here
Supportive shoes and orthotics
Pain from insertional Achilles tendonitis is often helped by certain shoes, as well as orthotic devices. Shoes that are softer at the back of the heel can reduce irritation of the tendon.
Heel lifts are also very helpful for patients with insertional tendonitis because they can move the heel away from the back of the shoe, where rubbing can occur. They also take some strain off the tendon. Like a heel lift, a silicone Achilles sleeve can reduce irritation from the back of a shoe. Further measures such as the use of a slant board, night splint and Strassburg sock are covered in the calf tightness section here.
If your pain is severe, Mr Davda may recommend a walking boot for a short time. This rests the tendon while keeping you mobile before any therapy is begun.
Extracorporeal shockwave therapy (ESWT)
During this procedure, high-energy shockwave impulses stimulate the healing process in damaged tendon tissue. ESWT is non-invasive and has minimal risk. Further details can be found here.

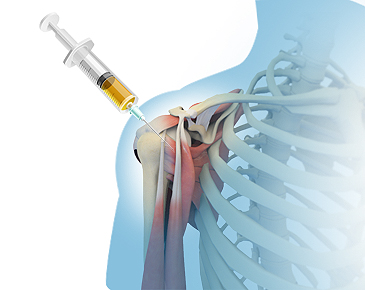
Platelet-rich plasma injection (PRP)
PRP is plasma with many more platelets than what is typically found in blood. The concentration of platelets and therefore the concentration of growth factors can be 5 to 10 times greater than usual. Injecting this into the tendons can accelerate its regeneration and therefore healing.
For a PRP preparation, blood must first be drawn from a patient. The platelets are separated from other blood cells and their concentration is increased during a process called centrifugation. Then the increased concentration of platelets is injected into the affected tendon. This is covered in greater detail here.
Surgical Treatment
Surgery should be considered to relieve Achilles tendinopathy only if the pain does not improve after 6 months of nonsurgical treatment. The specific type of surgery depends on the location of and amount of damage to the tendon. This will be discussed in greater detail with you by Mr Davda.
Surgical options include:
- Calf muscle release
This is a surgical lengthening of the calf (gastrocnemius) muscles. This allows the calf muscle to stretch, resulting in a greater range of movement to the ankle and less tension on the Achilles tendon itself. This is covered in greater detail here.
- Debridement of the Achilles tendon
The degenerative tissue is excised followed by a repair (when less than 50% of the tendon is damaged).
- Debridement of the tendon with tendon transfer (when the tendon has greater than 50% damage).
If the Achilles tendon is highly damaged and degenerate, it cannot effectively function. The tendon is detached from the heel bone and the degenerate areas removed. The tendon to the big toe (called the flexor hallucis longus) that runs alongside the Achilles is transferred to the heel bone to help restore function. The Achilles tendon is then reattached to the heel bone using bone anchors and stitches. This helps your ability to walk and lift yourself on tiptoes.
Recovery
Postoperative immobilisation is required in a cast and then boot for a period of six to eight weeks. This is followed by the gradual introduction of range of motion and strengthening exercises under the supervision of a physiotherapist. It may require 6 months to achieve full recovery. Complications of surgery include recurrence, stiffness of the ankle, and deep vein thrombosis. This will be discussed in greater detail with you by Mr Davda.
