
Ankle Arthrodesis Surgeon in High Wycombe, Buckinghamshire, Elstree
Ankle conditions like severe end-stage arthritis and ankle infections or instability may not respond to conservative treatment measures (medications or injections). In such cases, bones that form the ankle joint are fused using a surgical procedure called ankle arthrodesis to relieve the pain. Precision Foot and Ankle, Orthopaedic Surgeon, High Wycombe, Buckinghamshire, Elstree provides diagnosis and arthrodesis of ankle in High Wycombe, Buckinghamshire, Elstree. Precision Foot and Ankle, Orthopaedic Surgeon, High Wycombe, Buckinghamshire, Elstree also provides highly specialised care during and after the surgery. Contact Precision Foot and Ankle, Orthopaedic Surgeon, High Wycombe, Buckinghamshire, Elstree’s team for an appointment today!
- Request an Appointment
- Secretary
- HCA Esltree
- BMI Shelburne
- BMI Chiltern
What is ankle arthrodesis?
Ankle arthrodesis, commonly referred to as ankle fusion, is a surgical procedure employed for the treatment of ankle arthritis.
What is ankle arthritis and how is it caused?
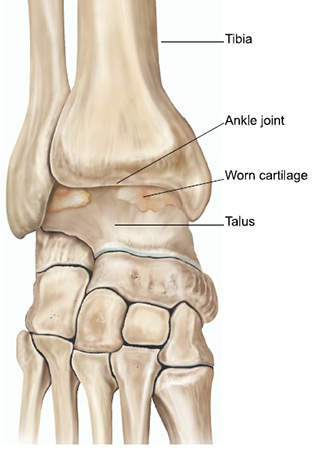
Osteoarthritis is often referred to as ‘wear and tear’ arthritis where the cartilage of the joint gradually wears down exposing the bone underneath. This can cause be a painful condition accompanied by progressive deformity. In the ankle, it often occurs in the years following a fracture, dislocation or ligament injury. Other causes of ankle arthritis include rheumatoid arthritis, flat or high arched feet, and neuromuscular conditions that can affect the walking pattern.
What are the symptoms?
Most people with ankle arthritis complain of one or more of the following: pain and swelling, which is worse during or after weight-bearing activity; loss of movement/flexibility in the ankle; difficulty walking on stairs and a limp.
Assessment
Your symptoms and a medical examination will determine the type of treatment that will be most appropriate for you. Conditions such as rheumatoid arthritis and diabetes may be present and affect the method of treatment your surgeon provides.
X-rays of the affected ankle are required so that the severity of the arthritis in the joint can be assessed. The surgeon may arrange a CT or MRI scan to further determine the course of treatment.



The x-rays above show the various patterns of arthritis that occur. The cartilage between the shin bone and ankle bone is worn.
What treatment is available?
Nonsurgical
There are many ways of reducing the pain caused by arthritis of the ankle without needing surgery. For example:
- Painkillers e.g. paracetamol, anti-inflammatories (discuss with your GP)
- Restriction of activity: avoiding long walks or running, for example
- Orthoses (braces or insoles)
- Footwear adjustment e.g. shoes with cushioning, boots that lace up above the ankle
- Walking aids e.g. crutches or a walking stick
- Injections of steroids are occasionally helpful in delaying the need for surgery. There is no evidence-based guideline as to the maximum number of injections one can have into the ankle joint, but in general, we would advise having no more than two injections every 12 months. The steroids act locally within the joint and do not have the systemic effects that are associated with taking tablets. Further information on the use of foot and ankle can be found here.
- Remedies such as glucosamine or chondroitin have not been shown to reduce arthritis or joint pain.
Surgery
The decision to have surgery is primarily based on whether you have pain that interferes with sleep or activities that you usually perform during the day. When this pain cannot be controlled by medication or other conservative measures, it is appropriate to consider surgery.
The aim of ankle fusion is to remove the arthritic joint between the shinbone (tibia) and ankle bone (talus). The worn cartilage is removed and the underlying fresh bone exposed. The bone surfaces are brought together and compressed typically using several large screws. Over the course of several months, the two bone surfaces knit together and ‘unite’. This turns a stiff painful joint into a stiff painless joint.
Ankle fusion is considered the gold standard procedure for ankle arthritis. It has a 95% success rate. Despite the fusion, patients will retain as much as 50% of normal up and down movement in the foot, because many of the joints in the mid and forefoot are still mobile. As the ankle joint is no longer painful, limping and walking pattern should improve. Indeed, many patients are able to go on long walks, cycle and even golf.
Before surgery
Your fitness for surgery and your ankle symptoms will be reassessed in our pre-assessment clinic, which takes place prior to the date of operation. Blood tests, as well as further investigations of the heart and lungs may be required to ensure you are fit to have a general anaesthetic. If you live alone, we will liaise with your GP and social services to ensure that care is in place to look after you following surgery. Occasionally, you may need to spend a few extra days in hospital whilst the services are being organised.
We kindly ask that you contact us if you suffer an insect bite, cut or bruise to the symptomatic leg in the period leading up to your surgery. Any injury to the skin in the area of your intended surgery can increase the risk of infection. You may need reassessment and surgery reorganised for another time.
On the day of surgery
You will be seen in the morning by Mr Davda or a member of the team to check your consent and mark the leg. Ankle fusion usually takes several hours and is commonly performed under general anaesthetic. Local anaesthetic is also applied at the time of surgery to provide pain relief and numb the foot. This can last for up to a day after. The anaesthetist will discuss this further with you on the day of surgery.
You will be in hospital for 2-4 days and will not be discharged until your post-operative pain is under control and the physiotherapists are satisfied with your mobility.
The Operation
In most cases, ankle fusion is performed using keyhole surgery. This involves making two small cuts on the front of the ankle, which allows passage of a small camera and surgical instruments. Occasionally, if a severe deformity of the ankle is present or the joint too narrow to pass a camera, a single larger incision is made at the front of the ankle. The worn cartilage is then removed, the ankle joint aligned and fixed together with screws. These are passed through a small cut made on the inner border of the lower leg. An x-ray machine is used at the time of surgery to ensure the screws are in the correct position. It is sometimes necessary to also use a plate. A cast is applied at the end of the operation and will normally stay on for three months. It will be changed periodically to ensure it is not loose and fits well.
After The Operation
The ankle will feel numb from the local anaesthetic for the first few hours following surgery. We encourage you to take painkillers as soon as possible, as the numbness will gradually fade over time. It is not uncommon for the wound to bleed and stain the cast, particularly when standing for the first time after the operation. The cast and dressings will be changed accordingly.
You will need to have a blood-thinning injection every evening for the duration of time in the cast, typically 3 months. You or your carer will be shown how to do this on the ward by the nursing staff.
For the first two weeks following surgery, you are advised to elevate the leg on 2-3 pillows, above the level of the chest. This will help reduce the swelling in the ankle and promote healing of the wounds.
Will I able to walk after the operation?
Your leg will be in a cast for the first three months following surgery. The typical weight-bearing regime is as follows:
Month 1 (0-4 weeks): strictly no weight through the operated ankle.
Month 2 (4-8 weeks): some or minimal weight through the operated ankle.
Month 3 (8-12 weeks): full weight bearing is permitted.
You may require a longer period in the cast if the ankle is slow to unite or you have an underlying condition such as diabetes.
Before you leave the hospital, our physiotherapists will show you how to walk with crutches or a frame.
You will be seen by Mr Davda or a team member in the post-operative clinic at about 14 days following surgery for a wound check and removal of stitches. Further appointments will be made in the months after surgery with x-rays taken to ensure the fusion is healing. Once the cast is taken off, you may be placed into a walking boot and physiotherapy will begin.


The x-rays above show a united ankle fusion from the front and side. Two screws have been inserted to hold the shinbone to the ankle bone in the correct position.
Commonly asked questions
When can I drive?
Patients having had the left ankle operated on will be able to drive an automatic car within 2-3 weeks (short distances only to avoid swelling). Those who have had an operation on the right side will be able to drive after about 12 weeks. You are advised to contact your insurance company to ensure you are covered to drive.
You are advised not to fly after surgery for six weeks (short haul) and 12 weeks (long haul).
When can I go back to work?
This will depend on the type of work you do. For example, if you have a desk job you may be able to return to work after two weeks provided you are able to rest and elevate your foot whilst sitting. If you do a physically demanding job, you will need a minimum of 12 weeks off.
Can I play sport?
The ankle will be pain free following fusion. You will be able to walk on the flat, slopes, cycle and play sports such as golf. Engaging in vigorous games such as football and racquet sports is unlikely. Walking on uneven ground can feel difficult.
COMPLICATIONS OF SURGERY
Ankle fusion has a success rate of about 95%, as with all surgery, complications can occur.
Swelling
This is very common after surgery. It is a side effect, rather than a complication, and can take up to a year to recover. You may need a shoe size slightly larger than you normally wear during this period.
Infection
This can occur in a small percentage of patients. If this is the case, it is possible that further surgery may be required to remove infected bone or screws. Minor infections are common and normally settle after a short course of antibiotics.
Numbness and tingling
This occurs at the surgical site, as a result of minor nerve damage and usually recovers over the course of six months.
Nonunion
The bones fail to join together. If you smoke, your risk of nonunion or major complications is greatly increased. It is therefore essential that you stop smoking before surgery and refrain from smoking until all bones have healed.
Malunion
Some ankles do not fuse in the exact position intended. This may be either due to the fact that the position was not achieved at the time of surgery or that the bones have shifted while in the cast.
Prominent metalwork
Prominent screws that can be felt through the skin or cause irritation may be removed at a later stage, typically a year after the initial procedure. Metalwork is not removed unless it is symptomatic.
Blood clots
A clot in the calf of the operated ankle (known as deep vein thrombosis or DVT) or a clot in the lung (known as pulmonary embolus or PE) is rare. Please inform the team if you have had a DVT or PE before, or if you have a family history of clotting disorders.
